Many of my patients with an autoimmune disease have asked if it puts them at a higher risk of contracting COVID-19 or developing more serious complications if they were to get COVID-19. Other patients worry if their autoimmune disease puts them in the immunocompromised category of individuals that need to take extra precautions. Not all individuals with an autoimmune disease are immunocompromised, however, certain medications used to treat some autoimmune diseases can be immunosuppressive.
There are several medical terms being discussed in the news and many types of autoimmune conditions – which makes understanding your particular risk factors difficult. Because this virus is so new there is not a lot of research to go on, so medical experts are advising that most people with autoimmune conditions should consider themselves at higher risk. But not all autoimmune conditions carry the same risk – some may not carry any increased risk at all. In order to help guide whether you may be at any more of a risk for developing COVID-19 or having adverse reactions to this virus, let’s break down some medical terminology and look at specific autoimmune conditions and commonly used medications.
Some medical terminology:
- Autoimmunity: When the immune system attacks its own cells and tissues.
- Immunosuppression: The partial or complete suppression of the body’s immune system.
- Coronavirus: a common human respiratory infection – it has been around for centuries. Many strains of coronavirus can cause symptoms associated with the common cold.
- COVID-19: “Corona Disease 2019” – “CO” stands for corona, “VI” represents virus, “D” stands for disease, and 19 signifies the year it was discovered.
- SARS: Stands for SARS-CoV (Severe Acute Respiratory Virus) and has not circulated since 2002-2003. This was the first SARS virus seen in humans. SAR-CoV had a higher mortality rate than SARS-CoV-2.
- MERS-CoV: a strain of the corona virus that causes respiratory symptoms and appeared in the middle east in 2012.
- SARS-CoV-2: this is what we are dealing with right now. It has a lower mortality rate than SARS-CoV but is unique in that it is highly contagious in individuals who have no symptoms.
Autoimmune Conditions and Specific COVID-19 Findings and Recommendations
Hashimoto’s Thyroiditis
Good news here, there is no indication that patients with Hashimoto’s thyroiditis are at a greater risk of getting COVID-19 or being more severely affected if they were to acquire the infection.
Rheumatoid Arthritis
Kevin Winthrop, a specialist in infectious disease epidemiology at OHSU School of Medicine in Portland, Oregon, stresses that there is still so much we do not know about COVID-19. He reports that people with rheumatoid arthritis (RA) who have a high disease activity are at increased risk of COVID-19 due to immune dysregulation. Many experts believe the greater concern is not so much the COVID-19 virus but the possible secondary bacterial infections that can follow the original viral infection. One thing to keep in mind is that medications used to treat rheumatoid arthritis may cause the immune system to be lowered, thus making someone more susceptible to any infection, including COVID-19 (a list of immunosuppressive drugs are listed below). Also, the medication hydroxychloroquine, often used in patients with RA is being investigated as a potential COVID-19 therapy – so could individuals with RA taking this medication have a protection? We do not know for sure. The good news, though, is that rheumatoid arthritis has so far not been reported as a high-risk condition increasing the chances of getting COVID-19 or having more severe reactions.
Lupus
Individuals with Lupus are considered to have an increased risk of catching infections in general and COVID-19 is not an exception. Like rheumatoid arthritis, individuals with lupus may be taking medications that lower overall immune response, making someone more susceptible to infections and developing more severe adverse reactions.
Inflammatory Bowel Disease (IBD)
IBD includes both Crohn’s and Ulcerative Colitis, which affect the health of the digestive tract. Both of these conditions are due to an overactive immune system and are often treated with immunosuppressive medications like steroids, which can increase an individual’s risk for contracting viral infections. There is not much research available looking at IBD and COVID-19, but the overall consensus is that if your symptoms are under control, you do not have an increased risk for getting COVID-19 or experiencing more severe reactions.
Type 1 Diabetes (and also type 2 diabetes)
Individuals with diabetes are considered to be more vulnerable to infections and to experience more serious complications. This increased risk is due to the fact that elevated glucose and insulin levels can impair the immune system. Current research, however, says that if individuals with diabetes have well managed blood sugar and insulin levels, they are not at a higher risk of contracting the Coronavirus. Experts also say that if someone with well managed diabetes does develop COVID-19, they are not at higher risk of developing serious complications.
Multiple Sclerosis (MS)
According to the national MS society, multiple sclerosis does not increase the risk of getting COVID-19. However, if you have MS in addition to other risk factors for developing COVID-19, MS may increase your risk of complications. These other risk factors are:
- Age 65 or older
- Chronic medical conditions, such as lung disease, heart disease, diabetes, cancer, and smoking
- Significantly restricted mobility – such as needing to spend most of your day in bed or seated
- Severe obesity or BMI over 40
- Living in a long-term facility
- Taking medications that suppresses the immune system
The National MS Society reports that if you do get COVID-19, it may cause a flare-up of your MS symptoms, but that these symptoms settle down once the infection clears.
Celiac Disease
There are currently no studies or reports suggesting individuals with celiac disease are at increased risk of contracting COVID-19 or of developing a more severe reaction to COVID-19. However, there is likely an increased risk in those with celiac disease who are experiencing malnutrition and weight loss, or those taking immunosuppressive medications. So, again, like the other autoimmune conditions listed above, so long as celiac disease is controlled, an individual is not at any increased risk of contracting or developing an adverse reaction.
Here is an overview of medications often used to treat autoimmune diseases. Please do not stop any of these medications without speaking with us or your doctor. Stopping these medications may cause more harm to your body than the increased risk of COVID-19 and some of these medications need to be discontinued slowly.
Drugs NOT considered immunosuppressive and do not increase COVID-19 risks:
- Thyroid medications (Levothyroxine, Liothyronine, Synthroid, Tirosint, Nature Throid, Cytomel, WP Thyroid, Armour)
- Mesalamine (Asacol HD, Pentasa, Delzicol, Lialda, and Apriso)
Medications that do lower the immune response:
- Steroids (prednisone): Steroids are immunosuppressive. Those on steroids should talk with their doctors to see if it makes sense to lower your dose or begin the weaning process.
- Biologics (Humira, Cimzia, Stelara, Remicade) do increase risk of infections.
- Immunomodulators – Methotrexate can slightly lower the immune response to viral infections. – JAK inhibitors (Xeljanz, Olumiant, Rinvoq) carry a slightly higher risk of catching infections.
The reality is that there is so much we don’t know about COVID-19, but, overall, I think the news is promising. If your autoimmune condition is under control and you are not taking medications that suppress your immune response, it appears your risk is not much different than anyone else’s. At Akasha, our goal is to get you to a higher level of health while building up your immune system and addressing the underlying root causes of autoimmune disease, such as gut microbiome, inflammation, and diet. Reach out to us if you have an autoimmune disease and you want to understand your specific risk factors and ways to enhance your immune system.
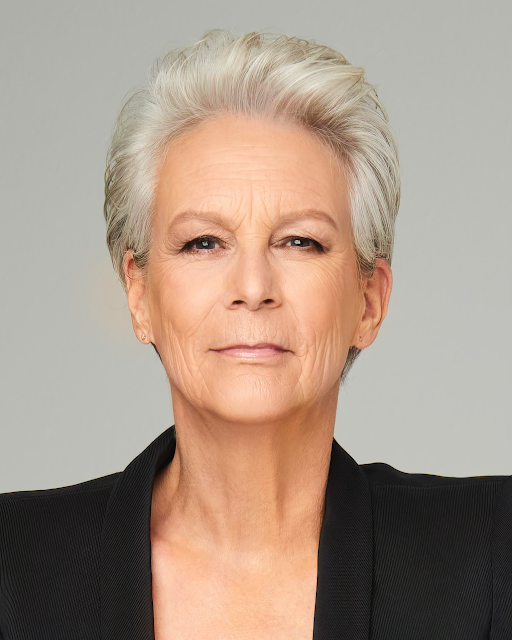
Dr. Maggie Ney is a Naturopathic Doctor and Director of the Women’s Clinic at Akasha. She specializes in hormones and health aging. You can make an appointment by calling 310-451-8880 or emailing us at info@akashacenter.com.