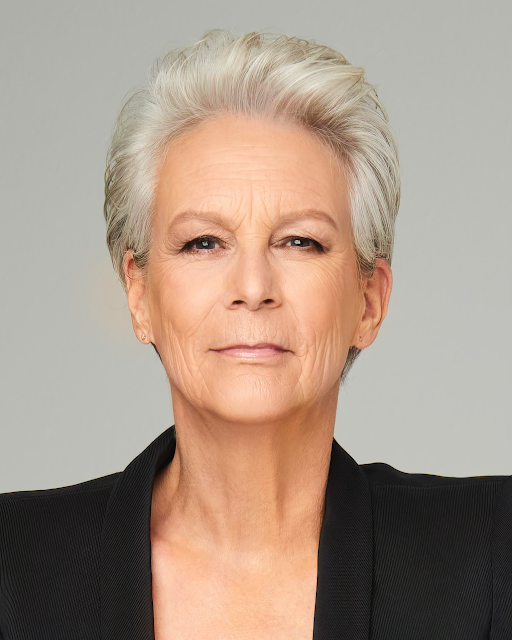
By. Bren Boston, MD
Medical doctors monitor your health with both bone density scans and coronary artery calcium (CAC) score scans. Have you wondered if the calcium supplements you take to prevent or treat osteoporosis might be depositing in the walls of your arteries? If you have a family history of both heart disease and osteoporosis and feel confused as to whether you should take calcium supplements, then congratulations you are not alone!
Fortunately, there are reasonable and effective ways to balance treatments for heart disease and osteoporosis.
Heart Disease:
Heart disease is the leading cause of death in the United States. One of the tests that doctors use to assess risk for heart attack is called the CAC score to measure calcium built up in the walls of the coronary arteries. According to the CDC, about 610,000 people die of heart disease every year in the US.
Osteoporosis:
Osteoporosis-associated fractures occur more than 1.3 million times every year in the United States. According to the National Osteoporosis Foundation, about half of women over age 50 will break a bone because of osteoporosis.
We are all familiar with the downward spiral that can happen after a hip fracture in the elderly. In fact, mortality rates double after hip fracture, and women ages 65-69 who break a hip are 5x more likely to die within a year than women of the same age who don’t break a hip according to a study funded by the National Institutes of Health.
Bone mineral density peaks at age 30 and decreases thereafter. The first step in the prevention or treatment of osteoporosis is adequate nutrition in regards to calcium and vitamin D. Vitamin D enhances intestinal absorption of calcium and phosphorus.
Research Suggests Dietary Calcium > Supplements:
Supplements – The research has been mixed as to the association of calcium supplements with heart disease. A 2013 study by the NIH suggests there is an increased risk of heart attack or stroke from taking calcium in men only. A 2016 Johns Hopkins study published in JAMA suggests taking calcium supplements may raise the risk of plaque build-up in arteries, although a diet high in calcium-rich foods appears to be protective. A Women’s Health Initiative (WHI) trial showed no effect of calcium and vitamin D supplementation on cardiovascular disease (CVD).
Dietary Calcium – In contrast to the concern raised with calcium supplements, prospective studies have shown either no relationship or a beneficial relationship between dietary calcium intake and risk of heart disease. Dietary calcium intake comes from dairy (milk, cheese, yogurt), dark leafy greens, broccoli, sardines, white beans, calcium-fortified foods like orange juice, tofu, and milk substitutes.
How can you tell if you are getting enough calcium in the foods you eat?
– There are several easy-to-use online calcium calculators such as on the International Osteoporosis Foundation website.
– The recommended daily calcium intake for postmenopausal women with osteoporosis is 1200mg (diet + supplement) and vitamin D is 1000IU. For pre-menopausal women, or men with osteoporosis, the recommended amounts are 1000mg Calcium and 800IU vitamin D. The National Osteoporosis Foundation considers supplementation in the dose range recommended above to be safe from a cardiovascular viewpoint.
If you calculate your dietary calcium intake and find that you fall short of the recommended daily values for calcium, what should you do?
– If you cannot increase your dietary calcium intake further, then you should use a calcium supplement to make up the difference. Your dietary calcium + your supplement should equal 1000mg per day for premenopausal women and 1200mg/day for postmenopausal women. Your total calcium intake (diet + supplement) should not exceed 2000mg/day because of possibility of adverse effects like kidney stones or cardiovascular disease. Other potential side effects of taking too much calcium include indigestion (dyspepsia) and constipation. In addition, calcium supplements interfere with the absorption of iron and thyroid hormone, and therefore these medications should be taken at different times.
– Calcium supplements can be most commonly found as either calcium carbonate or calcium citrate. Calcium carbonate is less expensive, but you have to take it with food to absorb it, and it is poorly absorbed if you are taking medication for heartburn. Calcium citrate is well absorbed in either the fasting state or with food, and is not affected by taking heartburn medications. Calcium supplements can only be absorbed 500mg at a time, so there is no reason to take more than 500mg in a single dose. Calcium-fortified foods are more like supplements than natural sources of calcium. They can vary in their bioavailability (how much you can absorb and use), but can be helpful for people who cannot tolerate dairy.
In summary, the best source of calcium for your health occurs in the foods you eat. You should use calcium supplements only if necessary to achieve the recommended daily amount of calcium and vitamin D. Supplementation in this dose range is considered safe from a cardiovascular standpoint.
–
Dr. Boston sees patients at the Akasha Center for Integrative Medicine at 520 Arizona Ave in Santa Monica, CA. You can make an appointment by calling us at (310)-451-8880 or emailing us at info@akashacenter.com