The scientific world is feverishly working to understand and treat the disease COVID-19, which stands for coronavirus disease 2019. The virus that causes this disease is called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The SARS-CoV-2 virus uses ACE2 receptors on the surface of cells as an entry route in many of our organs, not just lungs. The major morbidity and mortality from COVID-19 is due to an acute viral inflammatory pneumonia that evolves to acute respiratory distress syndrome. The most severe cases require assisted oxygenation either invasively using a ventilator or non-invasively using an oxygen mask. Other aspects to COVID-19 have emerged as causing significant health complications, including blood clot formation which can lead to a stroke or loss of a limb, and an overwhelming inflammatory syndrome called cytokine storm that can lead to organ failure.
There is no FDA approved cure for COVID-19, but strides have been made in how to treat patients leading to improved outcomes compared to earlier in the pandemic. Now it has been recognized that COVID-19 patients who are ill enough to require hospitalization will have improved outcomes if they are given a blood thinner to prevent blood clots. Blood thinners can prevent the strokes and loss of limb that were seen earlier in the pandemic before it was known that SARS-CoV-2 may cause blood clots.
Levels of a marker of inflammation in the blood called C-Reactive Protein (CRP) is measured in hospitalized patients, and when it reaches a level >=20mg/dL, then patients who are given intravenous dexamethasone (a steroid) have a reduced risk of needing mechanical ventilation. Patients who require ventilation do worse than patients who do not require ventilation, so preventing the need for ventilation improves the chance of surviving the virus. Giving dexamethasone when CRP is less than 10mg/dL worsens outcomes, so it is important that inflammation monitoring be guided by lab work and a physician. While steroids like dexamethasone can help when the patient is approaching a cytokine storm, if given too early, the steroid can dampen the patient’s immune response making them even more ill.
An antiviral medication called Remdesivir has been shown to result in a faster time to recovery. In patients who are not requiring ventilation, Remdesivir has been associated with a reduction in risk of death from COVID-19. More studies are ongoing to collect more information about how helpful Remdesivir really is for hospitalized COVID-19 patients.
Convalescent plasma is derived from the blood of patients who have recovered from COVID-19 and is rich in antibodies against SARS-CoV-2. Studies have suggested that when given early in the course of the disease, convalescent plasma has clinical benefit. Studies in patients with severe, life-threatening COVID-19 do not achieve a statistically different clinical outcome when given convalescent plasma despite the improved rate of viral RNA clearance they experience. Convalescent plasma is currently being studied for its use in prevention of COVID-19 in health care workers, and for prevention of worsening in mild and moderate cases of the disease.
Hydroxychloroquine/chloroquine is traditionally used to treat rheumatoid arthritis, lupus, and malaria. It has the potential to cause irregular heart beats, especially at higher doses. The data regarding its use in the treatment of COVID-19 are inconclusive, with lack of clear benefit while having potential for toxicity. Hydroxychloroquine is not being tossed out the window, as it is undergoing more clinical trials to determine whether it has a role in treating COVID-19 or not.
You might be wondering if you take the blood pressure medications called ACE inhibitors or ARBs would affect your risk for getting sick from the SARS-CoV-2 which uses the ACE2 receptor to enter cells. Studies so far have shown no protective benefit and no additional harm from taking these medications in relation to COVID-19. Therefore, unless there is some other reason to stop these medications, like if your blood pressure gets too low or your kidneys get sick, then you should continue your use of these medications as previously prescribed and directed by your physician.
Controlled inflammation is part of the early immune response to a germ. It is how your body identifies the foreign invader and tries to get rid of it. In some severe cases of COVID-19, an overwhelming syndrome of uncontrolled inflammation will occur called Cytokine Storm which makes your health worse rather than better. There are blood markers of inflammation that can be monitored in hospitalized patients to help predict if they are going to experience Cytokine Storm. Tocilizumab is a strong anti-inflammatory medication used for rheumatic diseases to reduce cytokine release and is being evaluated in clinical trials for treatment of COVID-19.
Nitric oxide is a molecule that opens arteries up wider to allow more blood to flow. If you inhale nitric oxide gas, then you can get more blood flow in the lungs and therefore more oxygen exchange. Nitric oxide also relaxes the air tubes called the trachea and the bronchioles, allowing more air flow to enter the lungs. Inhaled nitric oxide, not to be confused with laughing gas/inhaled nitrous oxide, is being studied in hospitalized patients to improve oxygenation.
Male gender has been found to be a risk factor for a worse outcome in hospitalized COVID-19 patients. There are ongoing studies with estrogen and progesterone to see if they play a role in the course of the disease. Estrogen is known to play a complex role in the early immune response of viruses in general. Topical estrogen patches are being studied to see if they will help hospitalized men and postmenopausal women, but results are not known yet. Progesterone helps fight inflammation and is being studied in hospitalized patients early in their course to see if it helps to prevent the need for oxygen or ventilation compared to a control group, and results are pending.
There are multiple active clinical trials occurring all over the world trying to figure out which combination of treatments, including many not named in this article, will help patients survive this disease.
There are many ways you can boost your immune system at home to help improve your chance of not getting sick. One important way is to avoid eating a lot of sugar, because viruses love sugar and thrive in a high sugar environment. Having diabetes or an increased blood sugar level has been shown to be a risk factor for a more severe course of COVID-19. Eating an immune-supportive diet that avoids sugar, flour, processed foods, and dairy, while doubling down on fresh veggies can improve your immunity and support the pathways in your liver that produce glutathione, one of our most important antioxidants. Immune supportive supplements like vitamin C, vitamin D, B-complex vitamins, zinc, NAC, garlic, Boswellia, and glutathione are helpful in boosting your body’s defense against germs. Getting 8 hours of sleep, regular exercise, wearing a mask when in an indoor public space, and connecting with your support network in socially distanced ways are all things you can control in keeping yourself healthy.
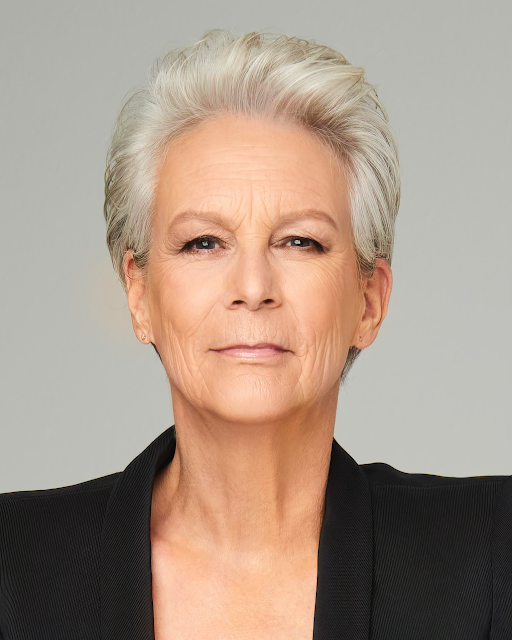
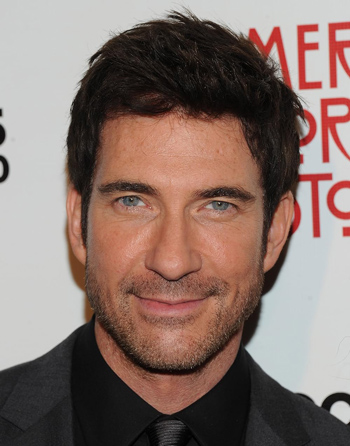
Dr. Bren Boston is a Medical Doctor at the Akasha Center for Integrative Medicine who specializes in Pain Management Sports Medicine and Women’s Health. You Can schedule an appointment with her by calling 310-451-8880 or emailing us at info@akashacenter.com